The Real Face
of Men's
Health
2025 United States Report
2025 United States Report



For more than twenty years, Movember has listened to men and those who care for them. We’ve heard stories of resilience, recovery, and deep struggle. We’ve talked to men who didn’t know their risks or feel equipped to act, and those who reached out for help, but didn’t find it.



But don’t just take our word for it. The findings in our Real Face of Men’s Health report feature new insights into national health data, as well as two large-scale surveys and the authentic voices of caregivers. Together, they paint a portrait of urgent challenges but also of practical, evidence-based solutions.

What we know is that every missed opportunity, barrier, and inequity has shaped stories of lives upended, and lost. Stories of men and those who care for them.
of
male
deaths
in the US
happen before age 75
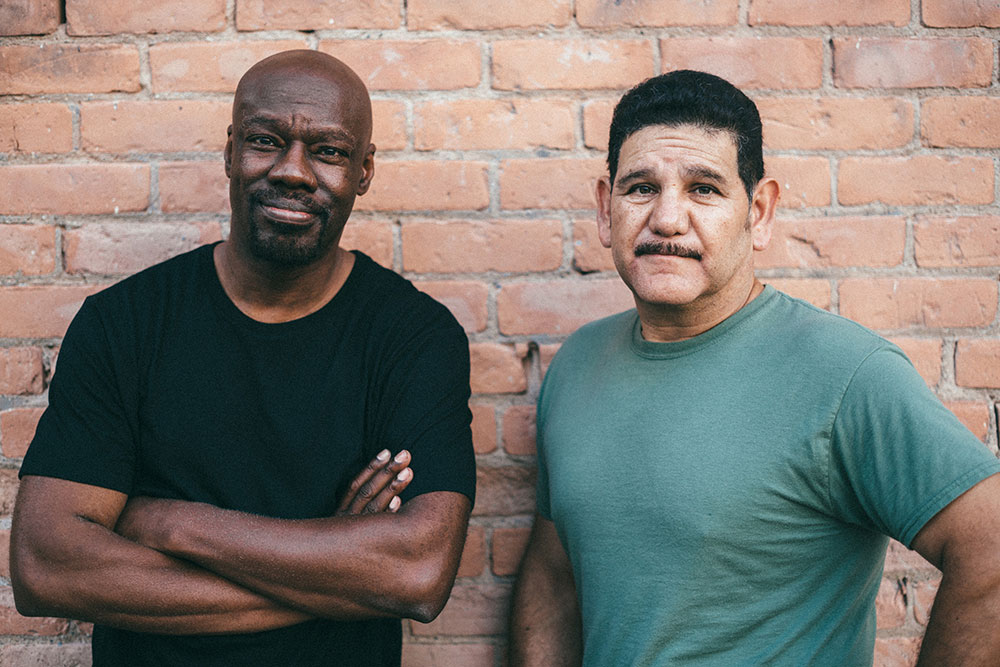
That’s not an arbitrary number: 75 years is the standard threshold for “premature mortality” in high-income nations such as the US – an age everyone should expect to reach in the absence of major health risks. But in the most recent year where data are available, the majority of male deaths were premature. In fact, men account for over three in five premature deaths nationwide.
This gap isn’t just about biology. It’s about systemic inequities in access to care, economic security, safe environments, and chronic stress. Even looking at boys born today, Black men and American Indian/Alaska Native men have never reached a 75-year life expectancy at birth. In these communities, premature death is the norm, not the exception.
This gap isn’t just about biology. It’s about systemic inequities in access to care, economic security, safe environments, and chronic stress. Even looking at boys born today, Black men and American Indian/Alaska Native men have never reached a 75-year life expectancy at birth. In these communities, premature death is the norm, not the exception.




 The sad truth: over 85% of these costs is considered preventable. If we were to save this
staggering amount, it would generate enough resources to fund the annual operating expenses
of over 1500 new hospitals – that’s 30 hospitals per state.
The sad truth: over 85% of these costs is considered preventable. If we were to save this
staggering amount, it would generate enough resources to fund the annual operating expenses
of over 1500 new hospitals – that’s 30 hospitals per state.
When men die too young, the loss is personal – years of connection gone, stories untold, families changed forever. This human cost is immeasurable. And the economic toll is staggering, too. In 2023, the five leading causes of premature mortality in men alone – heart disease, lung cancer, chronic obstructive pulmonary disease, suicide, and opioid use disorder – cost the US $120.8 billion in direct medical spending and $299.8 billion in lost productivity and wages.
of informal caregivers for men say their own mental health has suffered
say that caregiving deepens understanding and connection
Informal caregivers are the unexpected face of men’s health. Behind every story of illness or recovery is someone providing unpaid care – very often wives, mothers, daughters, or sisters. The strain is real. The work is invisible. The cost is high. Women caregivers in our study report net negative impacts across eight of nine areas of life, from personal time and energy to career and finances.

“It is an overwhelming issue and it has taken time to adjust and manage the stress and enormity of it.” - Woman, age 59, caregiver for spouse with cancer
But caregiving doesn’t bring just negative impacts. There are positive ones too. Over four in five caregivers say it leads to more quality time and deepens understanding and connection. Recognizing caregivers as central to men’s health policy isn’t optional, it’s essential.





When mental ill health rises to crisis levels, too many men are lost too soon. Suicide is the 4th leading cause of early death for men in the US, with the highest risks between age 25-34. Men are 3.6 times more likely to die by suicide than women. Without stronger social support and attention to mental health, more men will be lost, way too soon.
The fact is that mental health and social disconnection are driving crises, for men as well as women in the US. Anxiety, depression, and distress – compounded by social isolation – are escalating, made worse by loneliness. Loneliness itself is now considered a public health threat, comparable in impact to smoking or obesity.

of men agree that “taking care of your health is a sign of self-respect.”
say “avoiding regular check-ups is just part of being a guy.”
What it means to “be a man” still shapes health choices. In our new survey, most men say taking care of their health shows strength, and agree that it’s important to ask for help and support. At the same time, men also report feeling pressure to “push through pain” or skip preventive care.
This creates a gap between what men really believe and what they think others expect. The result? Silence and stigma. Closing this perception gap matters. It means more authentic connection, more support, and real change.




In sum: the real face of men’s health is not a single male patient in a clinic. It is the network of relationships and responsibilities that shape, and are shaped by, his health and well-being. By supporting men’s health as a shared concern – of families, workplaces, and communities – we create a healthier society for all.